We are delighted to share with you the highlights from the recently concluded 1st CSMC Cardiovascular Summit held last August 31, 2023 at 5th floor PCAS Auditorium. This event brought together leading experts and healthcare professionals in the field of cardiovascular health to discuss the latest advancements and updates in the post-pandemic cardiovascular world.
Organized with the aim to promote collaboration and knowledge sharing, despite the gloomy weather, the event was a bright success, attracting impressive speakers and enthusiastic attendees.
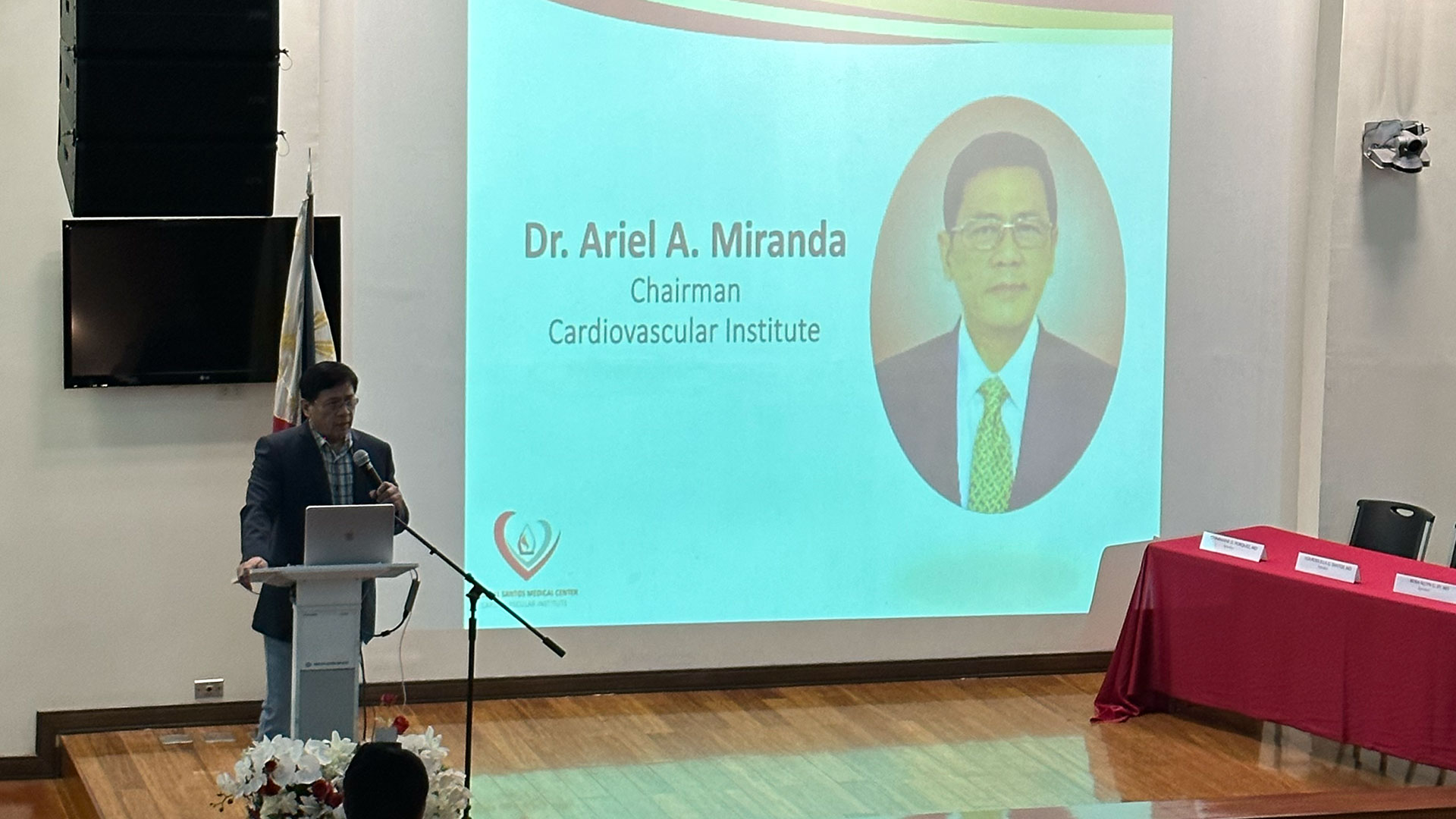
Hosted by Dr Michael Dela Cruz with opening remarks by Dr. Ariel A. Miranda and our CMO, Dr. Zenaida Javier-Uy

Breakfast Symposium: Promoting Cardiometabolic Wellness: Insights Into Prevention and Lifestyle Intervention
Moderator: Dr. Andrew Angelo E. Carreon
Speakers: Dr. Rosa Allyn G. Sy (Approaches in the Current Cardiometabolic State of Filipinos Post-pandemic), Dr. Lourdes Ella G. Santos (Current Goals and Treatment Advances in the Management of Hypertension and Dyslipidemia), and Dr. Charmaine DJ. Palafox-Porquez (Role of Cardiac Rehabilitation as Adjunct Treatment for Metabolic Syndrome)
Approaches in the Current Cardiometabolic State of Filipinos Post-pandemic
A comprehensive overview of diabetes remission and lifestyle intervention was presented. The concept of diabetes remission was discussed, emphasizing its potential for partial, complete, and prolonged abatement of the disease. The importance of early and aggressive intervention to prevent differentiation of pancreatic cells was highlighted, along with mentions of landmark trials and recent research that demonstrated the effectiveness of lifestyle interventions in glycemic and metabolic control. The recommendations from the American Diabetes Association (ADA) for achieving weight loss through lifestyle modification in individuals with prediabetes and diabetes were outlined. These recommendations encompassed dietary patterns, macronutrient intake, and strategies for managing comorbid conditions such as hypertension and dyslipidemia. Additionally, the role of meal replacements as effective tools within lifestyle intervention programs was discussed. The lecture highlighted the significance of structured weight loss programs, regular exercise, medical nutrition therapy, and pharmacological treatment in high-risk type 2 diabetes management. While ADA did not prescribe a specific eating pattern, it acknowledged that certain diets, like the Mediterranean diet or low-fat, low-carb options, may be beneficial. Furthermore, it was mentioned that very low-calorie diets (VLCD) using meal replacements could support short-term lifestyle changes, and long-term interventions with partial meal replacements might aid in achieving diabetes remission. Continuous monitoring was stressed as vital in preventing relapse. This lecture provided a comprehensive overview of diabetes remission, lifestyle interventions, and ADA recommendations for managing the disease, underscoring the importance of early and effective intervention in diabetes management.
Current Goals and Treatment Advances in the Management of Hypertension and Dyslipidemia
The lecture provided a comprehensive overview of the current goals and treatment advances in the management of hypertension and dyslipidemia, both of which are prominent and modifiable risk factors for cardiovascular disease (CVD). Increasing trends of modifiable risk factors and impact on CVD Development were discussed. The presentation highlighted the rising prevalence of modifiable risk factors such as elevated LDL cholesterol in the population, emphasizing their significant role in the development of CVD. This information was based on a local study, The ONE CAVITE Program, and the international 2021 ESC Guidelines on Cardiovascular Disease Prevention. The diagnosis and management of hypertension were tackled, referencing the ACC/AHA Guidelines, which advocates the use of combination therapy as a first-line approach. Additionally, it introduced the emerging role of sacubitril/valsartan in hypertension management and discussed the impact of telemedicine on hypertension care. The lecture also touched on factors affecting patient adherence to antihypertensive medications and mentioned landmark trials on renal denervation and its impact on blood pressure reduction. The presentation continued with a discussion on the diagnosis and treatment options for dyslipidemia. It covered different dosages and frequencies of therapies, including the mention of inclisiran, a subcutaneously injected PCSK9 inhibitor administered biannually. The lecture emphasized LDL cholesterol as the primary treatment target, non-HDL (including remnants) as the secondary target, and Lp(a) as a newer focus for treatment. Regarding the clinical benefits of LDL cholesterol lowering therapies, the lecture highlighted the significant clinical benefits of lowering LDL cholesterol, extending beyond statin therapy. It referenced the FOURIER trial as evidence of the effectiveness of these therapies. The presentation concluded by revisiting LDL targets and raising potential questions about non-HDL and Apo B 100-containing atherogenic lipoproteins as additional targets for evaluation and management.
In summary, the lecture provided an insightful overview of the current state of hypertension and dyslipidemia management, emphasizing their roles as modifiable risk factors for CVD. It covered diagnostic thresholds, treatment options, emerging therapies, and the importance of strict adherence to achieve treatment goals. The presentation highlighted the continuous advancements in cardiovascular risk management and the potential for improved patient outcomes.
Role of Cardiac Rehabilitation as Adjunct Treatment for Metabolic Syndrome
This lecture focused on cardiac rehabilitation as an adjunct treatment for metabolic syndrome. The outline covered the definition of cardiac rehabilitation, its components, and its benefits, including reducing mortality and morbidity in cardiovascular disease patients while improving various aspects of their health. The indications for cardiac rehabilitation were also highlighted, which included conditions like myocardial infarction, heart valve surgery, and heart failure. The connection between cardiovascular disease (CVD) and metabolic syndrome (MetS) was discussed, emphasizing that individuals with at least four out of five MetS features have a significantly increased risk of CAD and CVD mortality. The core components of cardiac rehabilitation were presented, showcasing its potential in addressing various aspects of MetS, such as fat mass, blood pressure, lipid profile, glycemic control, and inflammation. Several studies were referenced to support the positive effects of cardiac rehabilitation on MetS, including improvements in waist circumference, LDL-C, HDL-C, FBS, and blood pressure, with a notable 25% decrease in the prevalence of MetS. The discussion also covered the medical evaluation process for cardiac rehabilitation, exercise prescription, contraindications, and exercise types like aerobic and resistance training. Furthermore, the importance of factors like the talk test, rate of perceived exertion, diet and nutritional counseling, monitored exercise, educational programs, comprehensive medication reviews, smoking cessation programs, and goal monitoring in cardiac rehabilitation programs was highlighted. The presentation concluded by addressing barriers to cardiac rehabilitation and introducing the concept of home-based cardiac telerehabilitation as an alternative approach. In summary, the discussion underscored the role of cardiac rehabilitation as a comprehensive treatment option for metabolic syndrome, emphasizing exercise training and physical activity’s potential to improve various health parameters and clinical outcomes in individuals with MetS. Addressing barriers to cardiac rehabilitation was identified as crucial to maximizing its potential in treating metabolic syndrome.




Lunch Symposium: Rebuilding Hearts: Navigating and Conquering Heart Diseases After the Pandemic
Moderator: Dr. Mark David G. Fang
Speakers: Dr. Ariel A. Miranda (State of the Art: Physiology, Imaging and Intervention), Dr. John Andrew M. Yam (Minimally Invasive CABG and Hybrid Coronary Revascularization), and Dr. Rochelle Regina T. Cruz (Heart Failure and the Impact of COVID19 Pandemic)
State of the Art: Physiology, Imaging and Intervention
The lecture highlighted the evolving complexities in coronary physiology and imaging, challenging previously held beliefs in interventional cardiology. It began by discussing the limitations of traditional angiography, emphasizing that diameter stenosis alone is not sufficient to determine the significance of a lesion.
The historical reliance on angiography for assessing coronary artery disease, specifically focusing on the difference between diameter stenosis and cross-sectional area (CSA) stenosis was highlighted with the decision to treat a stenosis was traditionally based on the percentage of diameter stenosis, with 50% being considered significant. However, it was pointed out that this approach didn’t account for variations in flow due to lesion-specific factors, such as lesion length and eccentricity. The importance of coronary flow and lesion-specific factors in determining the physiological impact of stenosis was emphasized. The concept of flow and its relationship to stenosis severity was discussed, with a focus on Fractional Flow Reserve (FFR). FFR, with a cutoff value of 0.80, was introduced as a way to assess the physiological significance of coronary lesions, highlighting that it considers factors such as lesion eccentricity and geometry, which angiography alone cannot.
The lecture also touched upon the limitations of angiography in identifying functionally significant lesions and the importance of physiological measurements like FFR. The lecture stressed the underutilization of FFR in clinical practice, despite its proven benefits in improving outcomes and reducing costs in percutaneous coronary interventions (PCI). It also introduced the concept of non-hyperemic resting indices like iFR as an alternative to adenosine-induced hyperemia, reducing patient discomfort and procedural time. Furthermore, the lecture discussed the importance of combining intravascular physiology and imaging techniques in coronary interventions. It illustrated cases where angiography alone could lead to incorrect treatment decisions, while physiology and imaging together provided a more accurate assessment of lesions and treatment outcomes.
The lecture concluded by highlighting the synergy between revascularization and optimal medical therapy (OMT) in managing high-risk patients and lesions. It emphasized the need for a comprehensive approach that considers lesion severity, ischemia, and atherosclerotic burden to improve patient outcomes.
Overall, the lecture emphasized the evolving role of physiological measurements, such as FFR and iFR, in guiding coronary interventions, challenging traditional practices, and ultimately improving patient care and outcomes. It highlighted the need to consider both anatomy and physiology in the assessment and treatment of coronary artery disease.
Minimally Invasive CABG and Hybrid Coronary Revascularization
In the lecture, the audience was presented with an insightful discussion on cutting-edge advancements in cardiac surgery, focusing on two innovative procedures: Minimally Invasive Coronary Artery Bypass Grafting (MICS-CABG) and hybrid coronary revascularization (HCR).
MICS-CABG is a technique that departs from traditional open-heart surgery by utilizing small chest incisions or a mini sternotomy. This approach allows surgeons to operate on a beating heart, eliminating the need for a heart-lung machine. The lecturer emphasized the numerous benefits of MICS-CABG, including smaller incisions, shorter recovery times, reduced hospital stays, lower infection rates and improved cost-effectiveness. It was highlighted as an attractive option for patients seeking a quicker return to their normal activities and those at higher risk for traditional sternotomy. The indications for minimally invasive CABG were discussed, covering one to three vessel disease scenarios with good distal targets. The lecture also delved into four and five vessel bypasses through the MICS approach, although these cases were technically more challenging. Patients with previous inaccessible PCI or specific anatomical features were considered good candidates for minimally invasive bypass surgery.
HCR, a combination of angioplasty and bypass surgery, was introduced as an option for specific patient profiles, particularly those with proximal LAD stenosis and lesions in non-LAD vessels. The importance of a multidisciplinary approach, with thorough case discussions between surgeons and cardiologists, was emphasized to determine the best-suited procedure for each patient.
Throughout the lecture, the speaker conveyed a sense of optimism regarding the evolving landscape of cardiac surgery. The integration of minimally invasive techniques and the collaborative efforts of medical professionals were presented as promising factors that could significantly improve patient outcomes and enhance their quality of life, marking a notable shift in the approach to coronary care.
Heart Failure and the Impact of COVID-19 Pandemic
The speaker discussed the profound impact of COVID-19 on individuals with heart failure. The lecture delved into the ongoing symptoms that heart failure patients experience when they contract the virus, which encompass enduring challenges like breathlessness, weakness, and temperature fluctuations tied to their medical condition. Moreover, it was highlighted that heart failure patients tend to require unscheduled clinic or hospital visits even months after recovering from COVID-19, suggesting a lasting impact on their health.
The prevalence of cardiovascular complications among post-COVID patients was also emphasized, with a particular focus on heart failure. The intricate pathophysiology of these complications was explored, including potential direct viral effects on the heart and damage to endothelial cells leading to embolism. To address these challenges, a comprehensive diagnostic approach was advocated, encompassing various tests such as ECGs, biomarker assessments, echocardiograms, cardiac MRI, and stress testing. These tools were instrumental in confirming conditions like myocarditis and structural heart disease. Telemedicine emerged as a vital component in managing heart failure patients during the pandemic, allowing for the remote monitoring of vital signs and basic physical examinations through video calls. This approach not only enhanced patient safety but also promoted continuity of care. Lastly, the concept of a multidisciplinary heart failure clinic, designed to provide holistic care to these patients was also introduced. It involved specialists, caregivers, psychologists, and dietitians, aiming for a comprehensive approach to address the diverse needs of heart failure patients, particularly in the context of COVID-19.





Sunset Symposium: Delivering Excellence in Vascular Cardiology: Current Trends and Practices
Moderator: Dr. Michael Anthony A. Dela Cruz
Speakers: Dr. Ricardo D. Quintos (Multidisciplinary Management of CLTI), Dr. Maria Angela S. Cruz-Anacleto (Phlebolymphedema Unravelling the Connection), and Dr. Ma. Leonora B. Mendoza (Role of Venous Thromboembolism Prophylaxis Beyond the Pandemic)
Multidisciplinary Management of CLTI
Critical Limb Ischemia represents the End-stage of peripheral artery disease (PAD). It is a highly morbid disease, incurring significant mortality, limb loss, pain, and diminished health-related quality of life (HRQL) among those afflicted. The Global Vascular Guideline Standardization Framework promotes the use of the term CLTI, defined by the target population, to denote the universe of patients with advanced lower limb ischemia, wounds, neuropathy,and infection who are commonly referred to vascular specialists for evaluation and management. Men have been reported to have a higher prevalence of PAD in high-income countries whereas women seem to have a higher prevalence of PAD in low- and middle-income countries (LMICs), at least until age 60-64. Smoking, DM, hypertension, hypercholesterolemia, and air pollution are modifiable risk factors for PAD that are comprehensively studied. It is said that 5% of patients first presenting as claudication subsequently requiring intervention, and around 2% resulting in amputation and 30% of these patients will eventually succumb to cardiovascular events while 5-10% will experience nonfatal cardiovascular events. The clinical presentation of PAD ranges from the asymptomatic, intermittent claudication, ischemic rest pain, and gangrene. In ischemic rest pain, there is severe compromise of arterial flow. The pain is exacerbated by limb elevation, and relieved by dependency. If these symptoms are present, the condition is limb threatening. We can use the WIFI classification which correlates with the probability of limb salvage and wound healing after revascularization. The GLASS (Global Limb Anatomic Staging System) scoring targets arterial path and estimated limb-based patency and focuses on infrainguinal disease and infrapopliteal area. The importance of interdisciplinary teams and centers of excellence for amputation prevention is stressed as a key health system initiative and strategy that can be applied to treat CLTI.
Role of Venous Thromboembolism Prophylaxis Beyond the Pandemic
Deep vein thrombosis (DVT) and Pulmonary embolism (PE) known as Venous Thromboembolism (VTE) is associated with longer hospital stay and 10-15% mortality rate. The Virchow’s Triad formed by the venous stasis, vascular injury, and hypercoagulability are three elements that form the thrombus. VTE incidence is highest risk among medical patients. When the thromboprophylaxis is delayed, it is associated with higher mortality. We can use the Padua score in scoring non-surgical hospitalized patients who have potential risk of VTE. The IMPROVE bleeding risk score was designed to estimate the risk of bleeding in acutely ill hospitalized patients. Based on American Society of Hematology, thromboprophylaxis in acutely ill, pharmacologic therapy is recommended and LMWH or fondaparinux is the preferred. The ACCP guidelines suggest the use of mechanical prophylaxis in critically ill patients who are bleeding or at high risk for major bleeding using gradual compression stockings and intermittent pneumatic compression devices to prevent blood stasis and venous thrombosis in the legs. Major surgical procedures is also a risk factor for the development of VTE. Highest-risk procedures include invasive neurosurgery, total hip and knee arthroplasty, major vascular surgery. Total hip and knee arthroplasty have the highest incidence for DVT. Postoperative VTE can be reduced by the use of early ambulation, mechanical methods, and pharmacoprophylaxis. The Caprini risk score is a risk assessment tool for the occurrence of venous thromboembolism among surgical patients. For patients undergoing total hip arthroplasty or total knee arthroplasty, the ASH guideline suggests Aspirin or anticoagulants. When anticoagulants are used the panel suggests DOACS over LMWH, LMWH rather than warfarin or aspirin and LMWH over UFH. The OTTAWA and VIENNA models primarily determine VTE recurrence risk. The Khorana score is a well-validated tool that utilizes the following patient characteristics: Site of primary cancer, prechemotherapy platelet count, hemoglobin level, prechemotherapy count and BMI. The Ottawa score is a clinical prediction rule evaluating the risk of VTE recurrences during the first six months of anticoagulant treatment.
Phlebolymphedema Unravelling the Connection
Chronic venous disease is classified as primary, secondary and congenital. Primary is idiopathic, structural or functional parts of venous system and affects the venous wall and valve that leads to abnormal dilatation or weakness of the vein. Secondary venous disease are intravenous wherein vein damages occur, and extravenous wherein local hemodynamics are impaired due to external causes. Congenital venous disease cause venous hypertension and limb overgrowth. Age is one of the risk factors for developing CVD where the elder are the most susceptible. Female are more susceptible than men due to hormonal factors. Pregnancy is another risk factors wherein nulliparous women have 20% risk factor. Obesity causes an increase in abdominal pressure which may lead to increase vein reflux and vein diameter. Sedentarism is another risk factor due to deactivation of muscle pumps. The CEAP scoring is a tool for classification of CVD. Lymphema is caused by impairment of lymphatic drainage either through lymphatic abnormality or failure. Chronic lymphedema is edema persistent for atleast 3 months. When we examine a patient for limb swelling, we have to check for the Kaposi—Stemmer sign, which is due to high proteins in the insterstitium preventing redistribution. This is typically done on the 2nd toe. In acute lipodermatosclerosis, this may mimick cellulitis which presents with pain, redness, heat and swelling. In the chronic phase, the upside down champagne bottle appearance is seen. The venous ultrasound is the test of choice to check for the anatomical and functional of the venous system. The radionuclide lymphoscintigraphy is the test of choice to check for the function of the lymphatic system. The first step in the management of the lymphedema is the application of the compression. This may be in the form of bandages or compression stockings which not only improves hemodynamics but also flow of lymphatics. Complex decongestive therapy is recommended. This means after the compression. One of the most common medications given to lymphedema are diuretics. It is advisable to take diuretics that limit potassium secretion in the first 14 days with stable lymphedema with venous insufficiency. But diuretics is not useful for edema prophylaxis and is contraindicated in protein-rich fluid accumulation.




Special Lecture by Dr. Lucky R. Cuenza
Application of Cardiopulmonary Exercise Testing (PET) in Cardiology Practice: A Case Based Approach


The moderated poster presentation was held the 5th floor function room with our esteemed judges:
Dr. Eleanor A. Lopez, Dr. Dennis V. Sulit, and Dr. Anthony N. Lontoc with Dr. Raymond Banquirigo bringing home the bacon


Thank you to our main sponsors: Sanofi, AstraZeneca and Otsuka Pharmaceutical Co.

Thank you to our moderated poster presentation sponsor: Zydus Pharmaceuticals

It was indeed a fruitful event. See you on our next endeavors!